Introduction
The number of children and adolescents in this country who sustain traumatic brain injuries (TBIs) is staggering. A half million youngsters each year are taken to emergency rooms with head injuries from falls, motor vehicle accidents, sports, and abuse. Approximately 165,000 of these children will be hospitalized with 20,000 suffering moderate to severe symptoms.
TBI is the leading cause of death in children ages 0-4 and adolescents ages 15-19. Further, it is estimated that 145,000 adolescents ages 15-19 are living with lasting cognitive, physical, or behavior effects of traumatic brain injury (Center for Disease Control, 2015). Why are these numbers so high? The unique characteristics of the infantile, underdeveloped brain play a significant role.

The young brain is particularly susceptible to traumatic injury because:
1) brain neurons, and other structures and systems, are underdeveloped early in life leaving them more vulnerable to the acceleration/deceleration forces associated with head trauma; 2) immature brain neurons when traumatized tend to release excessive quantities of stored substances that create a toxic environment in the “extracellular space” of the brain leading to destruction of adjacent brain cells; 3) the skull segments in young children are still fusing and their skulls are much thinner; and 4) a child’s head is significantly heavier relative to the rest of its body, making small children particularly susceptible to falls that cause head and neck injuries. For these reasons and others, the same traumatic event can produce more severe outcomes in children than adults.
Diagnostic and therapeutic efforts are often complicated by the inability of a child to share what they are fully experiencing, further adding to the challenge. Equally problematic is the frequent reality that cognitive impairment in children from brain trauma may not surface for prolonged periods. Often, the full extent of injury only becomes apparent years later as the child gets older and faces increased cognitive expectations and new social challenges in more complex social circumstances. Though the injured brain has an amazing capacity to reorganize itself by forming new neural connections (plasticity), there are limits to this self-healing. Much debate exists on what those limitations may be in the pediatric brain. These factors, conditions, and others, make for a multitude of special medical and non-medical difficulties for both clinicians and parents, and of course, young patients.
Learning how best to confront these challenges begins with understanding the infantile nature of the brain at birth, the rapid structural developmental processes that occur in early years and beyond, and how during critical developmental phases a traumatic event can affect and sometimes alter the path to normal brain maturity. Awareness can help patients, parents, and families better understand and prepare for what may lay ahead.
Physiology…The Young Brain
We are born with 100 billion brain neurons (give or take a few million). As we grow older our brains do not create new ones. In fact, throughout life we lose brain neurons in the normal course of living, and unfortunately at times through disease and traumatic events.
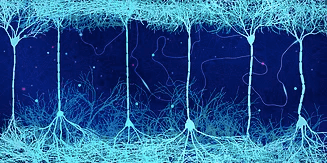
A brain neuron has its own unique cell structure consisting of three basic parts; the cell body or “soma” (which tells the neuron to send an electrical signal), an extended “axon” (through which the signal travels and exits), and “dendrites” (finger-like extensions that connect to other neurons) that pass the signal along.
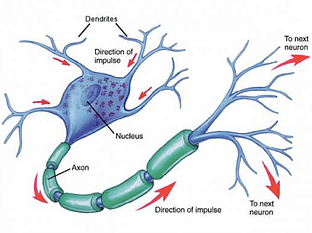
A single neuron standing alone can do nothing. Its purpose and function is entirely dependent on connections to other brain neurons. The connective network our neurons form makes possible all brain and body function. These connections called “synapses” vary over a person’s lifetime, but periods of massive proliferation occur in fetal development, infancy and adolescence. Thereafter, the brain undergoes equally massive bursts of “pruning” during which unused synapses are naturally eliminated by the brain.
At birth the brain of a baby has about 50 trillion neuron connections. That may sound like a lot, but not in comparison to the fully mature brain of an adult. When the brain neuron network is fully formed over 1,000 trillion connections will be made. Amazingly, by the time a child is one year old the full 1,000 trillion connections have occurred. Due to certain age-related structural conditions, however, these connections cannot function like they will later in life when the brain matures.
At birth and during early formative years certain regulatory systems in the brain are also not fully developed. When these immature systems under perform following trauma, significant brain tissue death can unfortunately occur.
Increased Susceptibility to Injury
Underdeveloped Neurons
All brain neurons are relatively delicate structures. At birth and during the early years, a child’s brain axons are particularly fragile and vulnerable because they lack an outer cover that serves to protect them. This protective sheath, which develops as a child grows older, is called “myelin” which acts as an insulating shock absorber when head trauma occurs. Myelin also serves the additional, critical role of facilitating the quick and efficient travel of electrical impulses through the nerve cell.
Myelination is a gradual process that actually begins in the brain stem and cerebellum before birth. It most rapidly develops in the first two years of life, but is not completed in the frontal cortex (the area responsible for executive function such as planning for the future, judgment, decision-making skills, attention span and inhibition) until late adolescence.
Until their axons are fully myelinated, children remain more vulnerable to the shearing forces of rapid acceleration/deceleration associated with head trauma simply because their neurons lack protective insulation.
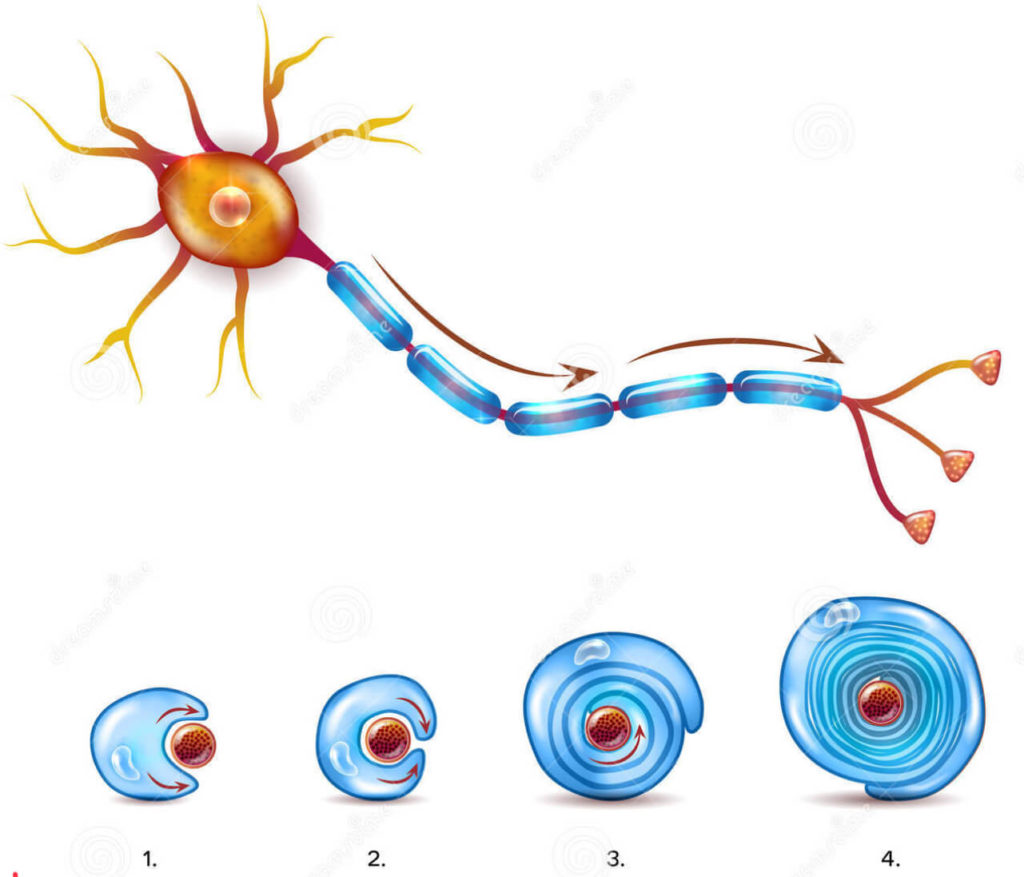
Lack of myelin in the early years also causes the brain to be less dense, more watery. When the brain becomes more dense, i.e., less watery, it can better absorb traumatic forces. When traumatic forces are applied to more watery regions of the brain where myelin has yet to develop, damage or more significant damage, tends to occur.
Brain Swelling
Here are the statistics. Diffuse (widespread) cerebral swelling frequently present in severe pediatric head injury is overall 2 to 5 times more common in children as in adults. Also, children have a higher incidence of increased intracranial pressure (ICP) following TBI than adults (80% vs. 50%). The immature brain is more susceptible to swelling from trauma for multiple reasons.
Increased swelling is believed to be the result of an underdeveloped auto-regulatory mechanism for cerebral blood flow (CBF) leaving children particularly vulnerable to uncontrolled “cerebral hyperemia” (increase in blood flow to the brain).
Since the cranial vault is incompressible and holds a fixed volume of brain matter, cerebral spinal fluid, and blood, any increase in one without a corresponding decrease in another can produce significant consequences through swelling and increased intracranial pressure (Monro-Kellie Hypothesis). The young, immature brain appears ill-equipped following trauma to automatically correct brain increases in volume to maintain the proper ratio of blood volume to cerebral spinal fluid.
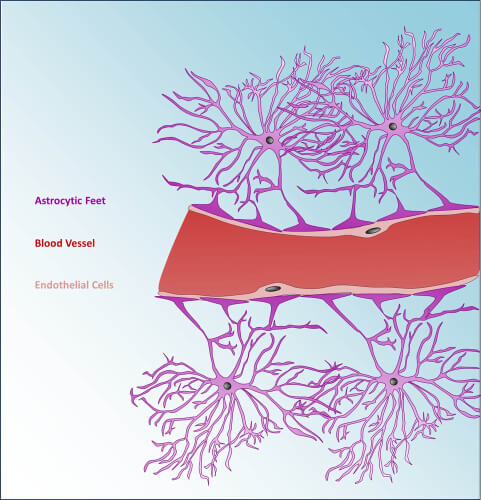
It is also believed excessive swelling in the young brain results from blood-brain-barrier disruption. This is referred to as “vasogenic edema.” The blood brain barrier (BBB) is a highly selective protective layer of cells lining certain blood vessels that helps prevent toxins (e.g., bacteria) traveling in the bloodstream from migrating into the brain.
When the BBB is damaged these toxins can enter the extracellular space and attack brain cells causing excess swelling, increased intracranial pressure and related brain tissue damage. It is widely held that developing cerebral vessels in children are more fragile than in adults, resulting in greater susceptibility to BBB damage and the higher likelihood of toxin “leakage” from traumatized blood vessels.
Greater Risk of Exitotoxic Injury
Excitotory neurotransmitters are present in the brain and are vital for neurotransmission and normal brain function. The most abundant of these is glutamate, which is stored in vast quantities inside brain neurons and only released during neurotransmission in very small amounts to allow a neuron to pass along a brain signal (action potential).
When traumatic forces are applied to the brain, delicate brain axons tend to shear and break causing an excess release of stored glutamate. When this happens a complex series of metabolic reactions occur allowing unhealthy amounts of calcium ions to enter damaged nerve cells resulting in cell death by “exitotoxicity.” Experimental studies have shown that the immature neurons in children are more susceptible to exitotoxic injury because calcium in elevated amounts is more difficult for the immature neurons to safely absorb. And, as referenced earlier, the unmyelinated neurons of a newborn and child are more susceptible to shearing-force injuries to begin with.
Unfused and Thinner Skull
Although the skull appears to be one large bone, there are actually several major bones that are connected together. The major bones that compose the skull of a newborn include two frontal bones, two parietal bones and one occipital bone. These bony plates cover the brain and are held together by fibrous material called “sutures.” Sutures allow the bones to move during the birth process. There are two spaces in the skull of a newborn that are not covered by bone but only by the cranial sutures. These spaces are called “fontanels,” or soft spots.
During the first two years of life, the separate bones of the skull slowly begin to fuse together. The fusing process occurs over multiple years because the brain is still growing and will not reach adult size until approximately age seven.
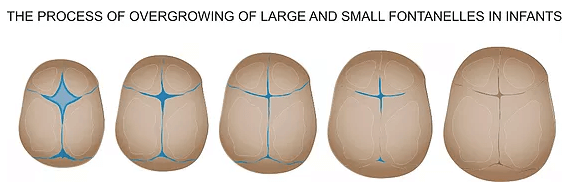
The two large soft spots on an infant’s head are closed by the time the child reaches age three. During these formative years a child’s skull is thinner, more fragile and lacks sufficient tencil strength and density to protect the brain like the skull of an adult.
Larger Head and Weaker Neck Muscles
Certain basic anatomical realities play a role in higher incidents of pediatric brain injury. For one, a child’s head is bigger relative to its body size than an adult. This tends to create imbalance leading to more falls. Combined with weaker neck muscles, a child’s head will tend to whiplash more than that of an adult causing greater brain movement inside the skull and greater damage as a result. Plus, children, particularly young children, are not as coordinated as adults, so again falls are more frequent.
What to Look For: Infant and Toddler Head Injuries
Infants and toddlers often lack the communication or developmental skills to overtly report the signs and symptoms of brain injury noted below. Clinicians and families need to be aware of the following signs that may be initially observed after head trauma for this age group:
- Changes in the ability to pay attention
- Changes in eating or nursing habits
- Changes in play (e.g., loss of interest in favorite toys/activities)
- Changes in sleeping habits
- Irritability, persistent crying, and inability to be consoled
- Lethargy
- Loss of acquired language
- Loss of new skills, such as toilet training
- Sensitivity to light and/or noise
- Unsteady walking, loss of balance
Take a child to the hospital emergency department immediately if they received a bump, blow, or jolt to the head or body, and:
- They have a headache that gets worse, and does not go away.
- They have weakness, numbness, or decreased coordination.
- They have repeated vomiting or nausea.
- They have slurred speech.
- They look very drowsy or cannot be awakened.
- They have one pupil (the black in the middle of the eye) is larger than the other.
- They have convulsions or seizures.
- They cannot recognize people or places.
- They get more and more confused, restless, or agitated.
- They have unusual behavior.
- They will not stop crying, and cannot be consoled or comforted.
- There is obvious distress with breathing.
- They lose consciousness (a brief loss of consciousness should be taken serious and the person should be carefully monitored).
Plasticity
Neuroplasticity, or brain “plasticity,” refers to the brain’s ability to change throughout life. The human brain has an amazing ability to reorganize itself by forming new connections between brain cells (neurons).
This occurs at the beginning of life when the immature brain first organizes and throughout adulthood whenever something new is learned and memorized. Brain plasticity also occurs in the injured brain to compensate for lost functions or to maximize remaining functions.
Whether children have the capacity to better recovery than adults from brain injury is to some extent debatable. Children have a wide range of functional outcomes from early insult making identification of specific recovery mechanisms elusive, and challenging to isolate and study. Children’s recoveries tend to represent extremes along a “recovery continuum.” Where a child’s outcome falls along this continuum depends on multiple injury factors and environmental influences, and the complex interplay between these numerous variables. Injury factors include severity, size, nature/type, site, related complications (e.g. seizures), age, and gender. Environmental influences include family stability/dysfunction, pre-existing neurobehavioral problems, sociodemographic factors, and access to interventional therapies.
On the whole, evidence is building on multi-levels of investigation—basic science, clinical neurology and behavioral sciences—to highlight the increased risk of morbidity following early brain insult, as compared with similar later insult. This elevated risk seems associated with the immaturity of the central nervous system generally and the potential that disruption will lead not only to direct, injury-specific insult, but will also derail on-going developmental processes. Contrary to this evidence; however, is a small and growing body of literature that demonstrates enhanced recovery post-early brain insult in a range of domains including: motor function (e.g. constraint-induced movement therapy), cognitive skills, (metacognitive training, use of compensatory aids), and social and behavioral function (individual psychotherapy, parent training).
Conclusion
Parents and patients should be heartened by knowledge that neuroscience research is intensely focused on pediatric brain injury with new breakthroughs occurring each year. Across the board in all types of brain injuries encompassing all age groups highly skilled and dedicated scientists, physicians, and expert therapists and counselors, are equipped now, more than ever, with advancing knowledge, and treatment protocols to help minimize deficits and maximize outcomes.
Stay safe out there!
-Charlie Waters